Digestive disorders affect millions—probably more than most of us realize. They can totally change how we eat, feel, and even how we plan our days.
Understanding these conditions helps us spot early warning signs and take steps to keep our digestive systems in better shape.
There’s a wide range here, from annoying heartburn to more serious stuff like Crohn’s or even colorectal cancer. The stomach and intestines can be a bit dramatic, honestly.
Sometimes we notice things like stomach pain, bloating, constipation, or diarrhea. But let’s be real, we don’t always know what’s causing it.
Learning about different digestive disorders and their causes can help us make smarter choices. If we have the right info, we’re more likely to manage symptoms, know when to call a doctor, and actually find treatments that work for us.
Key Takeaways
- Digestive disorders are common and can really mess with daily life.
- Recognizing symptoms and understanding risks matter for getting help early.
- Good management and the right treatment can make life a whole lot better.
What Are Digestive Disorders?
Digestive disorders happen when parts of our digestive system stop working quite right. They might involve the mouth, stomach, intestines, liver, or other organs, and the symptoms can really get in the way of everyday life.
At A Glance
Overview of the Digestive System
The digestive system—or GI tract, if you’re feeling fancy—starts at the mouth and ends at the anus. It includes the esophagus, stomach, small intestine, large intestine, rectum, liver, pancreas, and gallbladder.
Each part does its own thing: the stomach mixes food with acid, the small intestine grabs most of the nutrients, and the large intestine deals with water and waste. The liver, pancreas, and gallbladder chip in with bile and digestive enzymes.
So, if any of these organs aren’t pulling their weight, you might end up with digestive disorders. That can make digestion a pain—sometimes literally—and keep us from absorbing the nutrients we need for good health.
Want a deeper dive? Johns Hopkins Medicine lists out some digestive diseases.
Common Symptoms of Digestive Disorders
Digestive disorders can show up in a bunch of ways. Some of the most common symptoms are:
- Abdominal pain or cramping
- Nausea or vomiting
- Bloating or excess gas
- Diarrhea or constipation
- Heartburn or acid reflux
- Unexplained weight loss
- Blood in the stool
These can hit suddenly or sneak up over time. For example, GERD (gastroesophageal reflux disease) often means heartburn and can actually damage the esophagus over time.
Conditions like IBS, Crohn’s disease, and celiac disease can also mess with your digestive tract, causing pain, bloating, and a lot of unpredictable bathroom trips. There’s more on this at the Cleveland Clinic.
Prevalence and Impact on Health
Digestive disorders are everywhere—nobody’s really immune. GERD, IBS, and lactose intolerance alone affect millions every year.
Some conditions, like colorectal cancer or inflammatory bowel disease, are a whole lot more serious and even life-threatening. Chronic pain, missing work, or having to skip out on stuff with friends can really drag down your quality of life.
Long-term digestive issues can even lead to poor nutrition and more health problems. According to the National Institute of Diabetes and Digestive and Kidney Diseases, getting the right treatment early is key to avoiding bigger complications. Don’t wait until something small gets out of hand.
Major Types of Digestive Disorders
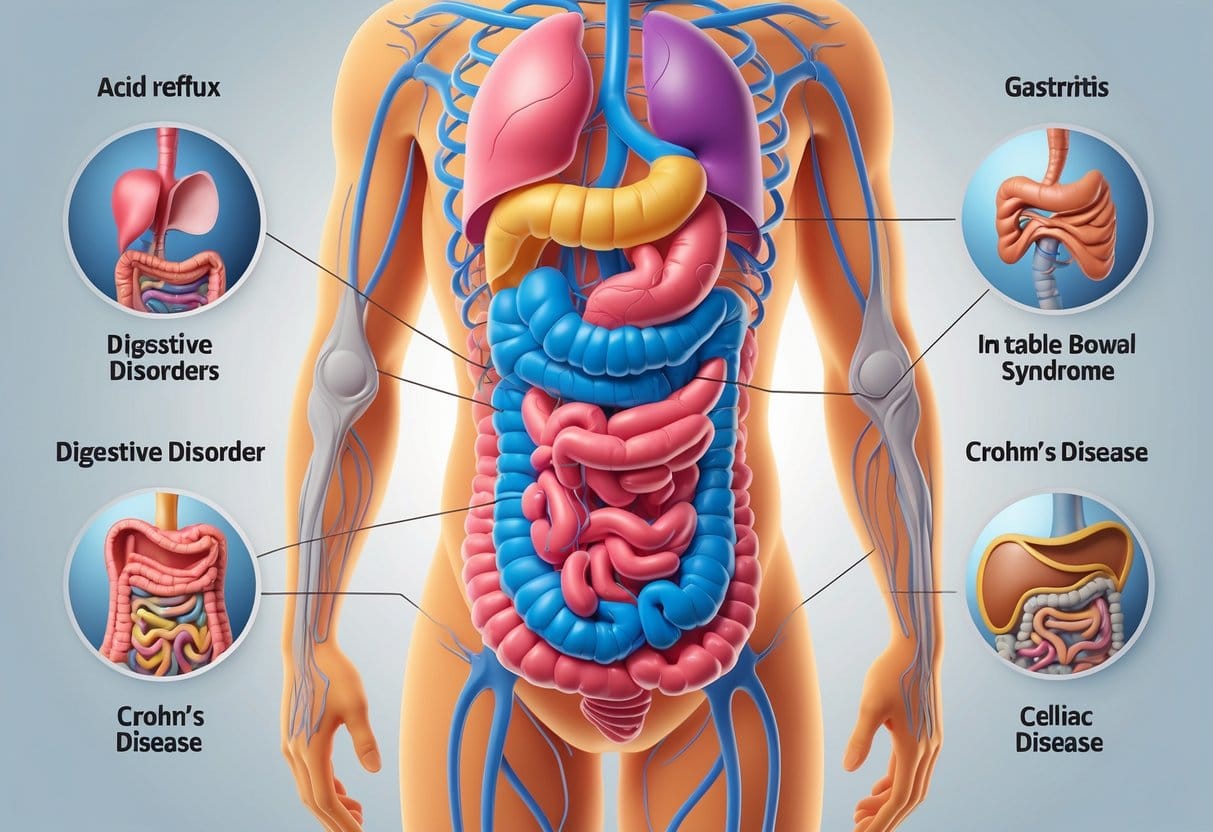
Digestive disorders show up in all sorts of ways, depending on which part of the gut is misbehaving. The type of disorder usually determines what symptoms you get—and what kind of treatment makes sense.
Functional Gastrointestinal Disorders
Functional GI disorders mess with how your digestive tract works, even though everything looks normal on scans or tests. The biggest example here is irritable bowel syndrome (IBS).
People with IBS often get stomach pain, bloating, and those fun swings between diarrhea and constipation. There’s no visible damage or inflammation, which can make it frustrating to diagnose.
Symptoms can be random—sometimes they flare up, sometimes they stick around. Treatment focuses on easing symptoms, tweaking your diet, managing stress, and sometimes using meds.
Other functional GI disorders include chronic constipation and functional dyspepsia. They’re annoying but not dangerous, usually getting better if you dodge trigger foods and keep your stress in check.
Inflammatory Bowel Diseases
Inflammatory bowel disease (IBD) is a group of disorders that cause long-term inflammation in the digestive tract. The two main types are Crohn’s disease and ulcerative colitis.
Crohn’s can hit anywhere along the GI tract, while ulcerative colitis sticks to the colon and rectum. Symptoms usually mean abdominal pain, diarrhea, fatigue, and weight loss. Blood in the stool isn’t uncommon, either.
Flare-ups can come and go, which makes life unpredictable. Treatment is usually about lowering inflammation with meds, but sometimes surgery is needed. Regular checkups are important, especially since long-term inflammation can raise your risk for colon cancer. There’s more about this at NIDDK.
Structural and Motility Disorders
Structural digestive disorders happen when the GI tract actually changes shape or gets damaged. Think Barrett’s esophagus (where the lining of your esophagus changes from acid reflux) or diverticulosis (little pouches in the colon wall).
If those pouches get inflamed, it turns into diverticulitis. Not fun.
Motility disorders are about how food moves through the system. GERD is one—acid sneaks back up into the esophagus, causing heartburn. Peptic ulcer disease is another, with painful sores in the stomach or upper small intestine, usually from bacteria or long-term use of certain painkillers.
Managing these depends on the cause—sometimes it’s lifestyle tweaks, sometimes meds, sometimes surgery. Here’s a good overview from UChicago Medicine AdventHealth.
Digestive Cancers
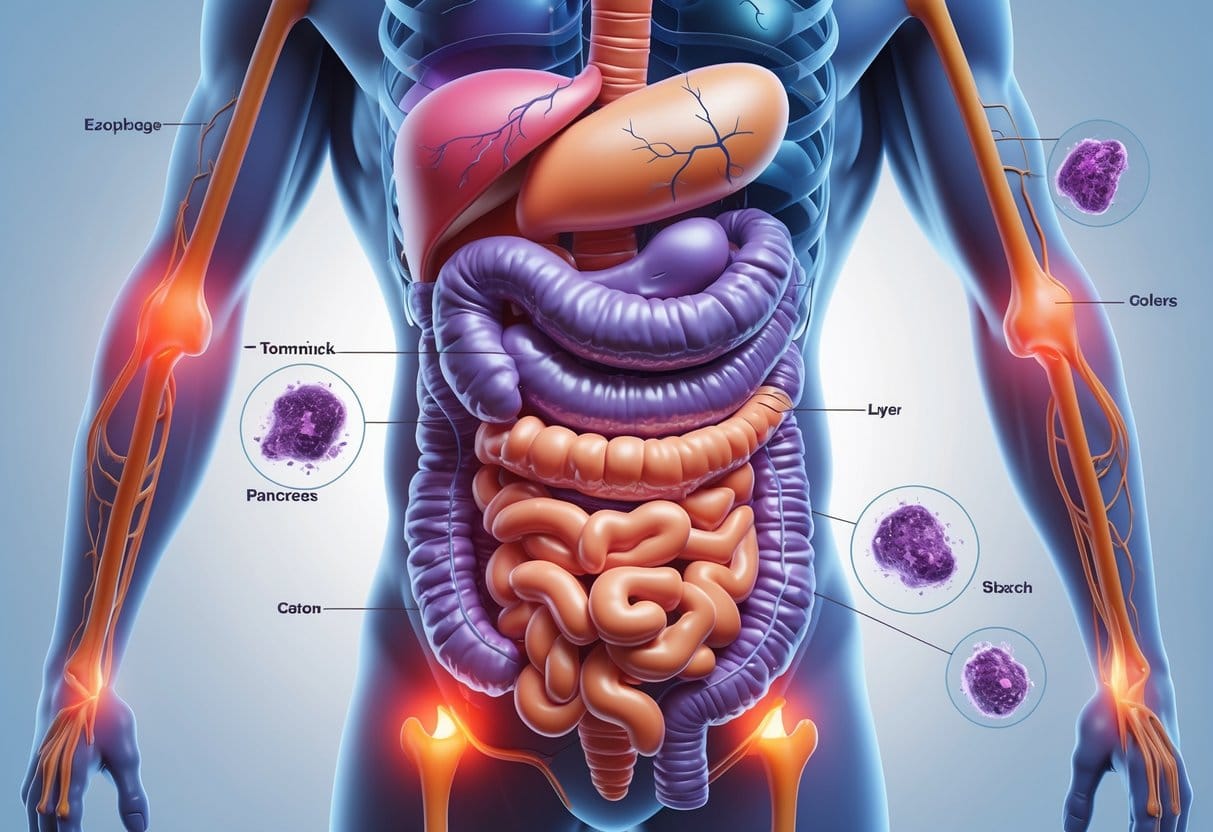
Digestive cancers can pop up in the colon, stomach, esophagus, pancreas—you name it. They can cause pain, mess with your eating habits, and are a real threat if you don’t catch them early.
Colon Cancer
Colon cancer usually starts with small growths (polyps) in the large intestine. Not all polyps are bad, but some can turn cancerous over time.
Signs to watch for: blood in your stool, unexplained weight loss, or changes in bathroom habits. Screening is crucial, since early colon cancer often doesn’t cause symptoms at all.
Doctors use colonoscopies to find and remove polyps before things get serious. Risk goes up if you’re over 50, have a family history, eat a lot of red meat, smoke, or have certain genetic conditions.
Treatment depends on the stage—usually surgery, chemo, and sometimes radiation.
Stomach Cancer
Stomach cancer forms when bad cells grow in the stomach lining. It can make swallowing tough, leave you feeling full after just a few bites, or cause bloating and stomach pain.
Some folks notice weight loss or nausea. Risks include H. pylori infection, eating lots of smoked or salty foods, smoking, and family history.
Early signs are often mild or easy to ignore, so it’s often not found until it’s advanced. Doctors use endoscopy and scans to check for it. Treatment usually means surgery, chemo, and sometimes radiation. Check the Mayo Clinic for more info.
Esophageal Cancer
Esophageal cancer starts in the tube connecting your throat and stomach. Trouble swallowing is a big red flag, usually starting with solids and getting worse over time.
Other symptoms: chest pain, choking, heartburn, vomiting, hoarseness, or coughing. Smoking, heavy drinking, untreated acid reflux, and Barrett’s esophagus all raise your risk. Weight loss can happen fast.
Diagnosis involves endoscopy, biopsy, and scans. Treatment depends on where and how much it’s spread—surgery, chemo, and radiation are common. More details are at the American College of Gastroenterology.
Pancreatic Cancer
Pancreatic cancer starts in the pancreas, which makes digestive enzymes. It’s tough to catch early—symptoms usually don’t show up right away.
When they do, you might see jaundice (yellow skin and eyes), belly pain, weight loss, and appetite changes. Risks include smoking, long-term diabetes, chronic pancreatitis, and some genetic factors.
Tumors can block the bile duct or press on other organs, causing pain and digestive problems. Diagnosis often uses CT or MRI scans, sometimes a biopsy.
Treatment is usually surgery, chemo, and radiation, but honestly, it depends on how far the cancer has spread. Pancreatic cancer is serious because it’s often advanced by the time it’s found.
Symptoms and Warning Signs

Digestive disorders show up in all sorts of ways, from pain and discomfort to weird changes in our bodies. Spotting a warning sign early can really help us dodge bigger problems down the road.
Abdominal Pain and Discomfort
Abdominal pain is probably one of the most obvious signs something’s off with digestion. The pain might be sharp, dull, cramping, or just a steady ache.
Sometimes it appears out of nowhere, or it lingers for days. Pain after eating is often tied to things like Crohn’s disease or peptic ulcers.
When pain keeps getting worse, interrupts sleep, or comes with fever or vomiting, it’s time to get checked out. Minor aches happen, but new or severe pain shouldn’t be ignored—better safe than sorry.
If you’re curious, here’s more about how pain connects to digestive disorders.
Changes in Bowel Habits
Bowel habits can really say a lot about digestive health. Some things to keep an eye on:
- Diarrhea lasting more than a few days
- Constipation that’s tough to manage
- Stool that’s black, tarry, or bloody
- Sudden urges to go
Long-term changes might point to irritable bowel syndrome, infections, or inflammation in the gut. Occasional changes are normal, but if it’s happening a lot, it’s worth paying attention.
Lasting changes—especially with pain, fatigue, or dropping weight—mean it’s probably time to talk to a doctor. Here’s a handy list of common GI symptoms if you want to dig deeper.
Gastrointestinal Bleeding
Bleeding anywhere in the digestive tract is a big red flag. It can show up in a few ways:
| Type of Bleeding | Appearance | Possible Causes |
|---|---|---|
| Vomiting | Bright red blood or dark | Ulcers, tears, cancer |
| Stool | Black, tarry, or red | Polyps, hemorrhoids, cancer |
Seeing blood—bright red, dark, or black and tarry—could point to issues in the esophagus, stomach, or intestines. Even if it’s not obvious, small amounts can add up, causing anemia or fatigue.
Heavy bleeding can lead to weakness or even fainting, so don’t wait around if you notice it. Any sign of blood is worth mentioning to your doctor. More details on the symptoms of GI bleeding are available here.
Unintentional Weight Loss
Losing weight without trying? That’s a pretty big clue something’s wrong—maybe your body isn’t absorbing nutrients, or there’s a more serious issue at play.
Conditions like celiac disease, Crohn’s, or certain cancers can cause this. Sometimes you’ll lose your appetite or feel full quickly, and weirdly, weight loss can show up before pain or other symptoms do.
If you drop more than 5% of your normal weight over six months (without dieting), that’s a sign to see a doctor. Unintentional weight loss, especially with other digestive symptoms, isn’t something to brush off. Here’s more about digestive disease warning signs.
Diagnosing Digestive Disorders

To figure out what’s causing digestive trouble, we typically use a mix of exams, lab work, imaging, and sometimes procedures. Getting a clear diagnosis means we can pick the most effective treatment for each person.
Physical Examination and Medical History
Understanding a patient’s symptoms and their health history comes first. During a physical exam, we’ll check the abdomen for tenderness, swelling, or odd noises, and look for things like skin changes or weight loss.
We’ll also ask about symptoms, eating habits, family history, and medications. These basics help narrow down what’s going on and guide what to do next. If you want more detail, take a look at Johns Hopkins Medicine.
Laboratory and Stool Tests
Lab tests help us spot infections, inflammation, or other issues. Blood and urine samples can check for anemia, liver function, or signs of disease.
Stool tests are useful for finding blood, infections, parasites, or inflammation. They’re especially helpful for things like diarrhea, chronic constipation, and unexplained stomach pain.
Some stool tests look for hidden blood (which can be a sign of polyps or cancer), while others check for bacteria or viruses. These tools usually point us in the right direction for the next steps.
Imaging Tests and Scans
Imaging lets us peek inside without surgery. Ultrasound, CT scans, and MRI can show blockages, growths, or inflammation, and sometimes a barium enema gives a closer look at the colon.
These scans help check the organs and tissues of the digestive system. Digital imaging can reveal problems that aren’t obvious from just a physical exam. For a deeper dive, see Johns Hopkins Medicine.
Endoscopic Procedures
Endoscopy lets us see inside the digestive tract using a thin, flexible tube with a camera. An upper endoscopy (EGD) checks the esophagus, stomach, and upper small intestine, while a colonoscopy looks at the colon and rectum for polyps, cancer, or inflammation.
Other techniques, like ERCP, examine the bile ducts and pancreas. Therapeutic endoscopy can remove growths or stop bleeding. Laparoscopy is a surgical option using tiny cameras to check the abdominal organs.
These procedures are done by a gastroenterologist and can diagnose—and sometimes treat—the problem right away. If you’re interested, MDHNGI explains more.
Contributing Factors and Risk Influences

Digestive disorders can crop up for all sorts of reasons. Risk depends on a mix of genetics, lifestyle, gut bacteria, and even how we’re feeling emotionally.
Genetic and Age-Related Risks
Some digestive problems just run in families. Inflammatory bowel disease and celiac disease, for example, have strong genetic ties.
As we age, our digestive tract doesn’t work quite as well—stomach acid drops, and intestinal muscles weaken. This makes things like constipation, acid reflux, or diverticulosis more likely.
Table: Age-Related Risks
| Age Group | Common Risks |
|---|---|
| Children | Food intolerances, celiac disease |
| Adults | Acid reflux, irritable bowel syndrome |
| Seniors | Constipation, diverticulosis, polyps |
Family history can tip the odds for some diseases even higher, especially when mixed with other risk factors.
Lifestyle and Dietary Influences
What we eat and how active we are really matters for digestion. High-fat diets, lots of processed foods, and not enough fiber can lead to constipation or heartburn. Overdoing spicy or acidic foods? That can irritate the gut, too.
Obesity ups the risk for things like nonalcoholic fatty liver disease and reflux. Alcohol and smoking damage the gut lining and raise the odds for ulcers or cancer. Not moving enough slows digestion, making constipation worse.
Sticking to a balanced, fiber-rich diet and staying active really does help. This guide on GI disease prevention covers it well.
Role of Gut Microbiome
The gut microbiome—all those bacteria and other critters in our intestines—plays a huge role in digestion, inflammation, and keeping out bad germs.
If the balance of gut bacteria gets thrown off, it can lead to issues like IBS, obesity, or even inflammatory bowel disease. Stuff like antibiotics, a poor diet, or infections can mess with that balance.
Eating more prebiotic fiber (think fruits, veggies, whole grains) and cutting back on processed foods can help keep things in check. Probiotics might help too, but it’s smart to check with your doctor before adding supplements.
Mental Health and Psychosocial Factors
There’s a real connection between our gut and our mind. Stress, anxiety, or depression can make digestive issues worse, or even trigger things like IBS. The “brain-gut connection” is no joke—a lot happens between the brain and intestines.
Chronic stress can mean more stomachaches, bloating, or bowel problems. And, honestly, digestive issues can make us feel more anxious or down, which just keeps the cycle going.
Coping strategies like counseling, mindfulness, or regular exercise can help break that cycle. Recognizing the mind-gut link might make it easier to manage both mental and digestive health, even if it’s not always simple.
Treatment and Management Approaches

Treating digestive disorders is rarely a one-size-fits-all thing. Usually, it takes a mix of medications, some dietary tweaks, maybe surgery, and regular check-ups to keep things in check.
The right approach really depends on the specific condition, your symptoms, and how severe things are. It’s not always straightforward, honestly.
Medications
Medications are usually the first thing doctors try for most digestive problems. They might suggest antacids for heartburn or proton pump inhibitors to cut down on stomach acid.
Antibiotics are common if there’s an infection, like H. pylori hanging around. For inflammatory bowel disease, anti-inflammatory meds or immune suppressors might come into play.
Irritable bowel syndrome? Sometimes that means antispasmodics or drugs for constipation or diarrhea. Probiotics can help balance gut bacteria, though results vary person to person.
Honestly, every medication should be handled by a gastro specialist. Side effects and weird drug interactions can sneak up on you.
Dietary Modifications
Diet’s a big deal for anyone dealing with digestive issues. More fiber can help with constipation, while cutting out dairy is a must if you’re lactose intolerant.
Celiac disease is a whole different ballgame—you have to avoid gluten completely. Eating smaller, more frequent meals can ease bloating or stomach discomfort.
For acid reflux, steering clear of spicy, fatty, or acidic foods usually helps. Upping your water intake makes digestion smoother and keeps constipation at bay.
It’s worth teaming up with a doctor or dietitian to figure out what actually works for you. Sometimes, even simple changes can make a surprising difference. These lifestyle changes are often super effective for functional GI issues.
Surgical Interventions
If meds and diet aren’t enough, surgery sometimes enters the picture. This might mean removing blockages or tumors, or dealing with damage from Crohn’s or colon cancer.
Stomach ulcers or gallstones can also land you in surgery. Severe ulcerative colitis may require removing part of the colon.
Surgeries range from quick endoscopies to more complicated operations. Deciding on surgery depends on your health, the disease, and what’s already been tried.
Gastroenterologists and surgeons work together to help you figure out the best move. It’s not a decision anyone takes lightly.
Long-Term Monitoring and Prevention
Managing chronic digestive diseases means regular monitoring—no way around it. That might involve check-ups, blood work, or imaging to catch changes early.
Colonoscopies are important, especially if there’s a family history or extra risks. Preventing flare-ups usually means sticking with a healthy diet, taking meds as prescribed, and avoiding known triggers like certain foods or stress.
Staying active and keeping a healthy weight can genuinely help your gut. Knowing the signs of trouble lets you catch problems before they get worse.
Quick action and early treatment can keep small issues from turning into big ones. Long-term monitoring really is a huge part of living well with digestive diseases.
Living With Digestive Disorders
Managing things like constipation, diarrhea, or bloating isn’t easy. These symptoms can mess with your daily routine and even relationships, honestly.
Coping Strategies and Support
Making life a bit easier starts with practical strategies. Eating small, balanced meals and keeping a food diary can help you spot which foods are troublemakers.
Staying hydrated and adding fiber to meals makes constipation less likely. Support from healthcare professionals is a must.
Talking with your doctor helps you understand what’s going on and what can actually help. Sometimes, counseling or joining a support group makes a huge difference, especially if stress or anxiety is making things worse.
Family and friends matter more than you might think. Honest conversations can take the edge off and help you manage with a bit more confidence.
Healthy relationships can even improve symptoms, according to research on digestive disorders and relationships.
Some everyday strategies that help:
- Eat slowly and chew food well
- Limit greasy or spicy foods
- Manage stress using relaxation techniques
- Get regular exercise
Long-Term Health Considerations
Living with a digestive disorder means long-term health is always on our minds. Some conditions, like irritable bowel syndrome or Crohn’s disease, can raise the risk of other issues if we’re not careful.
It’s smart to follow prescribed treatments, but honestly, it’s not always easy. When symptoms shift, seeing a specialist is worth it—even if it feels inconvenient.
Regular check-ups help our care team spot complications and tweak our plan as needed. Sometimes it’s a hassle, but it beats the alternative.
Sticking with healthy habits can really make a difference. Avoiding smoking and cutting back on alcohol? Not exactly fun, but both tend to make GI issues worse.
Stress is another big player here. It’s wild how much it can mess with digestion. Learning to relax—however you manage it—matters for improving our digestive health.
Paying attention to symptom changes lets us catch problems before they snowball. With all this, maybe we can actually feel a little better day by day.