Digestive disorders? Way more common than most folks realize. People of every age and background can get hit with them.
Symptoms like bloating, stomach pain, and heartburn might seem mild, but sometimes they’re a red flag for something bigger. Knowing the common signs and available treatment options gives us a shot at taking charge of our digestive health early—and honestly, that can make a huge difference in how we feel day to day.

Getting a handle on the different types of gastrointestinal disorders—from acid reflux and IBS to more serious stuff—equips us to spot issues and know when to get help. Staying informed and a little proactive really pays off.
For more details, check out some helpful guides on common digestive diseases and their treatments.
At A Glance
Key Takeaways
- Common symptoms may signal digestive problems.
- Treatments and healthy habits help manage most conditions.
- Early action supports better digestive health.
Recognizing Symptoms of Digestive Disorders
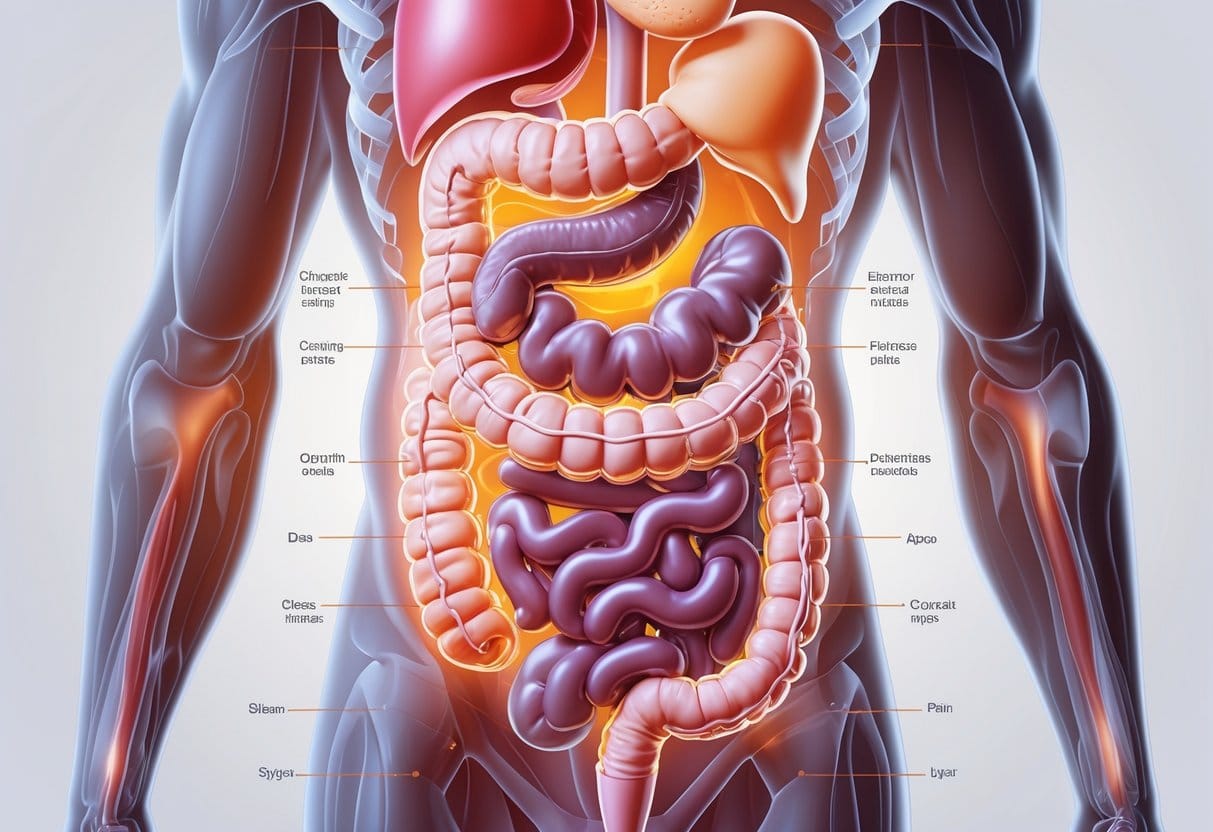
Digestive disorders can show up in a bunch of ways. Spotting the signs early gives us a better chance at getting the right treatment—and maybe dodging bigger problems.
Common Digestive Symptoms
Most digestive disorders come with a familiar set of symptoms. You might notice abdominal pain, bloating, heartburn, gas, or cramping—sometimes it’s just annoying, other times it really hurts, especially after certain foods.
Nausea and vomiting are also pretty common when your gut’s not happy. Episodes of diarrhea or constipation can pop up too.
If these changes stick around for more than a few days, it could be a sign of something like irritable bowel syndrome, acid reflux, or even inflammatory bowel disease. Other signs? Feeling wiped out even after sleeping or seeing blood in your stool—definitely not stuff to ignore. Read more about digestive disorders and symptoms.
Red Flags and When to Seek Medical Attention
Some symptoms just can’t wait. If you notice unintentional weight loss, long-term fatigue, or it’s suddenly hard to swallow, don’t put off calling a doctor.
Continued vomiting, black or bloody stools, chest pain, or ongoing diarrhea—those are big warning signs. Blood in vomit or stool, or chest pain with shortness of breath? That’s emergency room territory, no question.
Sudden, severe belly pain, strong cramping, or yellowing of your skin and eyes (jaundice) are also important to take seriously. These could be infections or bleeding that need fast attention. Learn more about red flag symptoms and when to seek help.
Impact on Daily Life
Digestive symptoms can really mess with your routine and mood. Ongoing bloating, cramps, or needing to rush to the bathroom might keep you home from work or social stuff.
Fatigue and pain can wreck your sleep, leaving you dragging through the day. Worrying about things like diarrhea or sudden vomiting? That’s enough to stress anyone out, and it can make you second guess what you eat or where you go. Stress is definitely part of the picture.
Dealing with digestive issues for weeks or longer can drag down your quality of life. Embarrassment, anxiety, frustration—they’re all common. Getting a proper diagnosis and treatment really does help people manage symptoms and feel more in control. More on this at Birmingham Gastroenterology Associates.
Overview of Common Digestive Disorders
Millions of people deal with digestive problems that can seriously interrupt daily life. Each condition tends to have its own symptoms, causes, and treatment options that can make a real difference.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a long-term issue affecting the large intestine. Symptoms can include cramping, gas, bloating, diarrhea, constipation, and changes in stool.
Usually, there’s no visible damage to the GI tract, but IBS can be uncomfortable and unpredictable. There’s no single cause—triggers might be certain foods, stress, or even hormonal shifts.
Managing IBS is all about figuring out personal triggers, tweaking your diet, cutting stress, and sometimes using medication. The good news? IBS doesn’t lead to more serious diseases, so treatment focuses on making life better. For more, check out this list of digestive disorders.
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD) happens when stomach acid keeps sneaking back up into the esophagus. The main symptom is heartburn—a burning feeling in your chest.
GERD might also cause regurgitation, chest pain, or trouble swallowing. Over time, untreated GERD can damage the esophagus lining.
Risk factors? Obesity, certain foods, smoking, and pregnancy top the list. Managing GERD usually means eating smaller meals, avoiding triggers, quitting smoking, and maybe propping up your head at night. Antacids help, but if they don’t cut it, prescription meds or even surgery might be needed. Learn more about GERD and treatment options in this digestive disorders article.
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease (IBD) involves swelling and damage somewhere along the digestive tract. The two big ones: Crohn’s disease and ulcerative colitis.
Symptoms can include belly pain, bloody diarrhea, fatigue, and weight loss. Crohn’s can hit anywhere from mouth to anus, often skipping around, while ulcerative colitis sticks to the colon and rectum in a continuous stretch.
Both are chronic and can get pretty rough, but medications help manage inflammation and symptoms. Sometimes, surgery is the best option. For an overview, see this digestive conditions guide.
Other Digestive Conditions
Celiac disease is the body’s over-the-top reaction to gluten, damaging the small intestine. People with celiac have to avoid gluten completely.
Peptic ulcers are sores in the stomach or small intestine lining, usually caused by H. pylori bacteria or long-term NSAID use. Gallstones can block bile ducts and cause sharp pain, nausea, or vomiting.
Diverticulosis means small pouches form in the colon wall, and if they get inflamed or infected, it’s called diverticulitis. Food intolerances—like lactose intolerance—are super common and can cause gas and stomach upset after certain foods. For a fuller list, check this digestive health resource.
Diagnosing Digestive Disorders
Figuring out digestive disorders usually takes a few steps. We use a mix of physical exams, lab work, imaging, and sometimes more specialized tests to get a clear answer.
Medical History and Physical Examination
At the first appointment, the healthcare provider will dig into your medical history. Expect questions about symptoms—pain, vomiting, diarrhea, constipation, appetite changes, that sort of thing.
Don’t forget to mention blood in stool, unexplained weight loss, or fevers that just won’t quit. During the physical, they’ll check your belly for tenderness, swelling, or odd sounds, and look for signs like pale skin or a fast pulse.
This step helps decide which tests, if any, come next. If things look serious or just keep coming back, you might get referred to a gastroenterologist.
Laboratory and Blood Tests
Lab tests are a big part of figuring out what’s up with your digestive system. Blood work can spot anemia, infections, or inflammation.
Low red blood cells can mean bleeding somewhere inside, while high white blood cells might mean infection or inflammation. Some tests also check liver or pancreas function if digestive symptoms are in play.
Stool tests come in handy too—they can pick up infections, parasites, blood, or absorption issues. Tests for Helicobacter pylori (via blood, breath, or stool) can help diagnose ulcers and gastritis. All these guide us toward the right treatment, or let us know if we need to dig deeper.
Imaging Studies and Endoscopy
Imaging studies like ultrasounds, X-rays, or CT scans let us peek inside without surgery. These can reveal swelling, blockages, growths, or organ problems that you just can’t see from the outside.
Endoscopy is a bit more direct—a thin tube with a camera goes down the esophagus, into the stomach, or through the intestines. It’s a great way to spot ulcers, inflammation, bleeding, or weird tissue. Sometimes, the doctor will grab a small tissue sample for more testing.
Colonoscopy is another go-to. The doctor looks at the whole colon for polyps, cancer, or the source of chronic symptoms. Both procedures help get a fast, accurate diagnosis. More info at this Cleveland Clinic article about gastrointestinal diseases.
Specialized Diagnostic Procedures
Sometimes, standard tests just don’t cut it. Breath tests can help spot lactose intolerance, Helicobacter pylori infection, or even small intestine bacterial overgrowth.
Capsule endoscopy is pretty wild—you swallow a tiny camera, and it snaps photos of your small intestine. This part of the gut is tricky to see with regular scopes, so it’s kind of a game changer.
Manometry tests measure how the muscles in your esophagus or intestines contract. They’re useful for diagnosing swallowing issues or certain motility disorders.
pH monitoring comes into play if we’re checking for acid reflux over 24 hours. It’s not the most comfortable, but it gives good info.
If symptoms don’t fit the usual suspects, your doctor might suggest genetic tests or more advanced imaging. These specialized tools help us get the right answers and start treatment that actually works.
There’s a full overview at Medical News Today’s list of digestive disorders if you want to dive deeper.
Treatment Options and Lifestyle Modifications

Managing digestive disorders usually means juggling a few approaches. Medical treatments, changes in what we eat, and sometimes surgery all play a part.
These strategies help control symptoms, cut down on flare-ups, and honestly just make life a bit easier.
Medication and Medical Therapies
Most treatment plans kick off with medication. Doctors might go with antacids for heartburn, anti-inflammatory drugs for Crohn’s disease, or laxatives if constipation is the main issue.
If there’s a bacterial infection, antibiotics can be prescribed. Other meds might target pain, cramps, or diarrhea—depends on what you’re dealing with.
Some folks need immune-suppressing drugs, especially if the body is attacking its own digestive tract, like in ulcerative colitis. Staying on top of regular check-ups is key to see if the meds are doing their job or if something needs tweaking.
Different problems call for different meds, so following your doctor’s advice is pretty important. Sometimes one medication does the trick, but often, a mix of therapies works best.
If you’re curious about treatment options, check out this overview on digestive disorders and therapy.
Dietary Changes and Nutrition
Food choices matter—a lot. For celiac disease, a gluten-free diet is non-negotiable.
Some people swear by a low-FODMAP diet to cut down on bloating and gas. High-fiber foods can help with constipation, though they might actually make IBS symptoms worse for some.
Trying an elimination diet can help pinpoint which foods set off symptoms. Keeping a food diary and tracking how you feel is surprisingly helpful for building a plan that works for you.
Hydration is easy to overlook but makes a noticeable difference for digestion. Water keeps everything moving.
Some digestive disorders mess with how well we absorb nutrients, so we might need extra vitamins or minerals, either from food or supplements. More nutrition tips are out there if you want to dig in.
Probiotics and Supplements
Probiotics—those good bacteria—can help balance things in the gut. You’ll find them in some yogurts and, of course, supplements.
They’re especially handy after antibiotics or during a flare-up. But not all probiotics are created equal, and honestly, it can be a bit of trial and error.
Other supplements like fiber, vitamin D, iron, or B12 might be recommended if you’re not getting enough from food. Some people need digestive enzyme supplements if their body can’t break down certain foods properly.
It’s smart to talk with your healthcare provider before jumping into new supplements. You want to make sure you’re getting what you need—without any unwanted side effects.
Surgical Interventions
Sometimes, when nothing else works, surgery is the next step. It can mean removing damaged sections of the digestive tract, fixing blockages, or dealing with emergencies like perforations or bleeding.
Common surgeries include appendectomy (taking out the appendix), cholecystectomy (removing the gallbladder), or colectomy (removing part of the colon). Inflammatory bowel diseases like Crohn’s or ulcerative colitis sometimes end up here if meds and lifestyle tweaks aren’t enough.
Surgery isn’t without risks—things like infection or changes in nutrient absorption can happen. But for some, it’s a real turning point for quality of life.
It’s worth having a detailed talk with your healthcare team about surgical options and what recovery might look like. If you’re considering this, here’s more info on surgical interventions for digestive disorders.
Managing and Preventing Digestive Disorders
Improving digestive health is all about the little things we do every day. Focusing on habits and handling stress in smarter ways can really lower the risk of common digestive issues.
Lifestyle Changes and Regular Exercise
Even small changes in our routines add up. Eating a balanced diet with plenty of whole grains, fruits, veggies, and lean protein helps digestion run smoothly.
Cutting back on processed foods, fatty meals, and added sugars can make a noticeable difference, especially for things like acid reflux and constipation.
Not smoking and keeping alcohol to a minimum also protect the digestive tract. Both habits can really mess things up if left unchecked.
Getting regular exercise—even just walking for 30 minutes most days—keeps things moving in the gut. Consistency is the secret sauce here, honestly.
Need more ideas? This digestive health guide is worth a look.
Stress and Anxiety Management
How we feel mentally really does affect our gut. High stress and anxiety crank up symptoms, especially in IBS and acid reflux.
Relaxation techniques help. Deep breathing, stretching, or meditation can calm the body and ease gut tension.
Sticking to a regular sleep schedule matters too. Bad sleep just seems to make everything worse, doesn’t it?
Setting aside even 10 minutes a day for something enjoyable—music, a quick walk, whatever works—can support both mental and digestive health. More on this mind-gut connection is in this digestive health resource if you’re curious.
Prevention Strategies and Healthy Habits
Prevention’s not a one-time thing—it’s an ongoing effort. We’ve got to actually listen to our bodies and schedule regular medical checkups.
That way, we can catch little issues before they snowball into something bigger. Sometimes it’s tempting to skip those appointments, but honestly, it’s usually worth the hassle.
Eating slowly, chewing thoroughly, and avoiding lying down right after meals all help with good digestion. And let’s not forget handwashing with soap—it’s such a simple thing, but it really does keep a lot of gut-wrecking infections at bay.
Here’s a quick checklist for digestive health:
- Eat meals at the same time each day
- Drink plenty of water
- Limit fried, spicy, or heavily processed foods
- Avoid unnecessary antibiotics
- Don’t ignore chronic symptoms
Sticking with these habits gives us a bit more control over our digestive well-being. If you want to dig deeper, check out this article on digestive disorders and prevention.